The USCOM and Inotropy.
Can we measure inotropy using the USCOM? You bet we can! And it’s surprisingly simple and quick to do. Let’s start with some very basic physiology (don’t I always?)
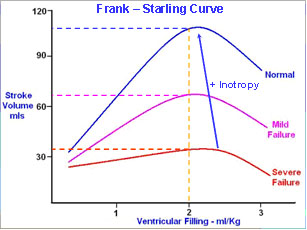
Preload is otherwise known as ventricular filling, or more specifically, that volume that is in the ventricle immediately before the onset of systole. This is the ventricular end-diastolic volume or VEDV, and can be right or left depending on the ventricle involved, giving us RVEDV and LVEDV. In the main, preload normally refers to LVEDV (and no, they are not always the same volumes on both sides!). The Frank-Starling curve shows that for any given preload, the stroke volume depends critically on inotropy. In ventricular failure where inotropy is low, stroke volume will also be low. Cardiac output and cardiac index will consequently be low unless the heart rate can increase considerably. In the three curves above, a threefold increase in heart rate would be required to maintain CO and CI as inotropy falls from the highest level to the lowest, as CO = Stroke Volume x Heart Rate. Stroke volume is at the very centre of haemodynamics, and inotropy is at the heart of stroke volume. Inotropy is therefore central to haemodynamics.
In adults with septicaemia the cardiac index is often high, being greater than 5 L/min/m2 during the phase when SVR is low. In the Bathurst Base Hospital series, the highest value we have seen was a cardiac index of 9.1 L/min/m2 in a patient with an SVR of 181 dyne.s.cm-5. As SVR increases in response to vasopressors, the CI can fall dramatically, and can fall to below 2.5 L/min/m2 well before the SVR reaches normal (around 800-1000). In short, vasoconstriction is precipitating cardiac failure. The ventricle has insufficient inotropy to maintain a normal stroke volume in the face of anything approaching a normal afterload.
The degree of myocardial depression in septicaemia ranges from around 25 to 60% in adult patients, but myocardial depression may not seem obvious when the cardiac output is 15 L/min! In these patients the ejection fraction can be 90%, but it does not mean that inotropy is high, far from it.
This shows the misleading nature of ejection fraction as an index of inotropy, implying that vasodilators have a positive inotropic action as stroke volume and ejection fraction increase with their use, while noradrenaline, which often leads to a lower stroke volume and ejection fraction, would appear to be a negative inotrope! Clearly we need to find a better way to assess inotropy.
Sophisticated echocardiographic techniques can give us some guidance and wall tension/stress and maximum acceleration indices are often used, but this requires considerable skill at echocardiography and is not practical in the acute setting of the ED or ICU, let alone out-patients or the doctor’s office. In a way, it is rather like analyzing the movements of the pistons and other components in the motor of a car to estimate the vehicle’s on-road performance. If you’re a Ferrari race engineer then it is possible, but very, very difficult.
We can turn this around though and say that if we measure the vehicle’s on-road performance we can deduce a lot about the power of the motor. How fast can it go on the flat? What speed can it maintain on a gradient? These are all direct functions of power. The power generated by the motor determines how fast a vehicle can climb a hill or its top speed on the flat. The power generated by the motor appears as potential energy and kinetic energy in the vehicle.
|