Hemodynamics: The Basics.
So what is hemodynamics? Essentially, it is the study of blood flow to the body tissues. All the tissues of the body need an adequate blood flow to deliver nutrients and oxygen and remove the products of metabolism. “Any circulatory disturbance leading to inadequate perfusion and inadequate oxygenation of the tissues” is as good a definition of shock as any, but cardiac failure, hypertension and hypotension even without inadequate perfusion all fall under the umbrella of hemodynamics. Is the patient's hypoxia due to a pulmonary or cardiovascular cause? Hemodynamics and the USCOM will tell you. Is the patient’s hypotension due to cardiogenic causes or vascular collapse? Again, hemodynamics and the USCOM will tell you.
Still interested? Then let's start with a very basic analogy between Ohm’s Law and the circulation.
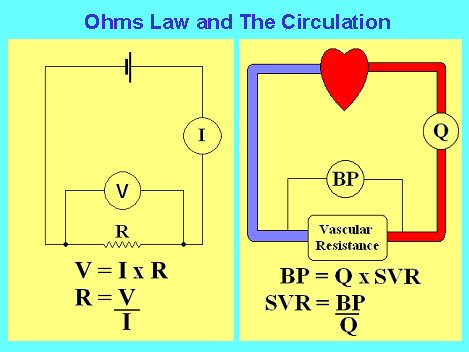
In the example on the left, we have a battery and a few wires coupled to a resistor. For a given current flow I, the voltage that is generated across the resistance is given by I x R. This is Ohm’s Law. In the example on the right, for any given blood flow, Q, the blood pressure that will be generated by this flow through the vascular resistance is given by the same formula, in this case BP = Q x SVR. In effect, Ohm’s Law works just as well for the circulation as it does for our simple circuit.
Blood Pressure.
There are only two things that can go wrong with blood pressure, it can be too high, hypertension, or too low, hypotension. From our simple analogy with Ohm’s Law we know that if the blood pressure is too low then it can only mean that the cardiac output is too low, the systemic vascular resistance is too low, or both are too low. Similarly, if the blood pressure is too high then either the cardiac output or systemic vascular resistance or both are too high. Simple.
Cardiac Output.
The cardiac output is the product of the stroke volume and the heart rate, so we could rewrite our simple formula as
BP = SV x HR x SVR
Now we know that the normal mean blood pressure is around 90 mmHg, a typical heart rate would be around 75 bpm, but how do we know the stroke volume and how do we calculate systemic vascular resistance?
The systemic vascular resistance can be calculated from the simple formula SVR = BP/CO. The problem of course is that we need to know the cardiac output in order to calculate the SVR, and to know the cardiac output we have to know the stroke volume. The USCOM measures cardiac output by first measuring stroke volume, which it does by measuring the ejection velocity of blood flow across the aortic or pulmonary valve and multiplying this by the cross-sectional area of the outflow tract diameter (OTD). It then displays the stroke volume directly on-screen. By calculating the interval between successive pulses the heart rate can be measured. Multiplying the stroke volume by the heart rate gives us the cardiac output. If we input the patient's blood pressure then the USCOM can calculate the SVR.
Returning to the simple model of hypotension and hypertension, we can now say that if the BP is too high then it could be because the heart rate is too high, the stroke volume is too high, or the SVR is too high, or a combination of these. Similarly for hypotension, the heart rate, the stroke volume or the vascular resistance is too low, or a combination of these. Let's examine some clinical examples of this, starting with hypotension. In the first category the BP is low because the cardiac output is low because the stroke volume is low.
BP low, CO low, SV low |
- Myocardial contractility low
- Conduction defects
- valvular heart disease
- Mechanical inefficiency
- "Toxic myocardium"
- Metabolic upsets
- Drugs, anesthetics
- Arrythmias
- Sub-optimal preload
|
Most of these you will be familiar with, but what exactly do we mean by "sub-optimal preload"?
|