Hypertension.
BP = CO x SVR
Again this simple formula derived from Ohm’s Law tells us that if the blood pressure is high then it can only be due to raised cardiac output, raised vascular resistance, or a combination of both. The treatment of hypertension then becomes entirely straightforward. If the cardiac output is high and the SVR is normal then we need to reduce the cardiac output. This is where diuretics and ?-blockers come into their own. If the cardiac output is normal but the vascular resistance is too high, then we need to use something that lowers the peripheral vascular resistance. This can be any one of the vasodilator drugs such as ACE inhibitors, Angiotensin Receptor Blockers (ARB’s), calcium antagonists or whatever. If the elevated blood pressure is due to a combination of both increased cardiac output and increased SVR then we need a combination of the two types of treatment, but how much of each? Again the answer is simple - that amount of each drug which reduces the cardiac output and the vascular resistance to normal. If both CO and SVR are normal then blood pressure cannot be anything other than normal.
If we contrast this with the way that the majority of hypertension is treated both in primary care and even in hospital outpatients, you're just as likely to end up on one particular drug as any other. Indeed it is highly likely that the drug that you will be prescribed is the one written on the side of the doctor’s (free) ballpoint pen! In the past this is about as logical as prescribing in hypertension has been.
With the USCOM we now have the ability to prescribe medication in hypertension in an entirely rational way based on the patient’s underlying hemodynamics.
These are the readings for a 72 year old female with hypertension (170/110), and angina, being treated with atenolol 50mg daily. What are your thoughts?
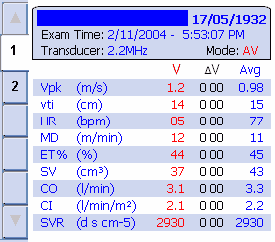
Clearly, her cardiac index is too low, whilst her SVR is sky high! Her AMD is only 11-12. It’s not surprising that her BP is high or that her heart is working hard against that sort of afterload. This patient is crying out for a reduction in her SVR which would both reduce her BP and her angina, and probably allow her CI to increase to a more normal value. It’s easy to add a vasodilator and re-evaluate her hemodynamics. Maybe she still needs a small dose of ?-blocker as well as an ACE inhibitor or calcium antagonist, time will tell, but we can monitor exactly how she responds to medication and fine-tune our therapy now. No more guesswork.
As a parting thought, have you ever considered how many hundreds of clinical trials of anti-hypertensive medication have been carried out involving probably millions of patients. How many of them ever considered the underlying pathophysiology or hemodynamics? Given this, how much can we rely on this vast and almost unchallenged body of work? Can we take morbidity and mortality studies that were performed as if all hypertension were the same and apply this to any individual patient whose hypertension is due to say, a high cardiac output? Is their risk the same as the patient who has a raised SVR and a normal or low CO? The answer is that we simply don't know and a vast amount of work lies waiting to be revisited, revalidated and completely re-evaluated!
|